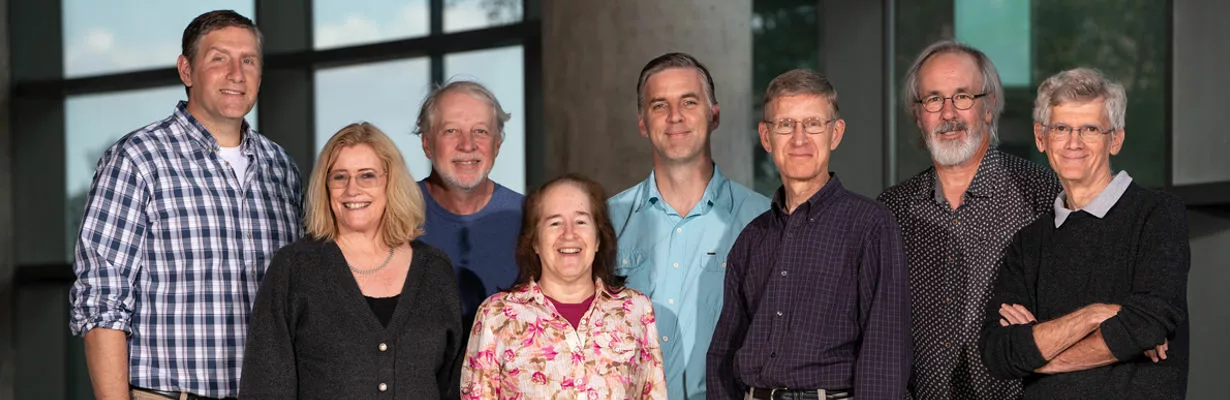
The program project grant’s five projects are conducted by eight team members, as follows:
- Project 1: Molecular Genetics of HPV Infection and Oncogenesis, led by Lambert with Ahlquist as a co-investigator
- Project 2: Mechanisms of HBV Virus Replication, led by Loeb with Ahlquist and Sherer as co-investigators
- Project 3: Characterizing the Amplification Factories of EBV and Kaposi’s Sarcoma- Associated Herpesvirus, led by Sugden with Johannsen as a co-investigator
- Project 4: Controlling the Latent-Lytic Switch in EBV, led by Mertz with Kenney as a co-investigator
- Project 5: EBV Drivers of Oncogenesis and Novel Therapies, led by Kenney with Johannsen and Sugden as co-investigators
In line with the program project grant’s goals to “understand the life cycles of human tumor viruses, identify their contributions to the induction and maintenance of human tumors, and develop novel approaches to prevent and treat these tumors,” the team focuses on three types of human tumor viruses — papillomaviruses, hepadnaviruses and herpesviruses — which contribute to 19 of the 21 viral-induced human cancers.
In progress reports, Lambert describes the grant’s seminal contributions. For instance, the team has trained more than 140 post-doctoral fellows, many of whom have established distinguished careers. Also, over the past five years, program project grant team members:
- published more than 90 papers that contribute to the global understanding of human tumor virus biology and ways to prevent or treat viral-associated cancers;
- discovered the critical role of estrogen receptor alpha expression in the stroma in mediating estrogen’s carcinogenic effect on cervical epithelia in mice and women, and the cell non-autonomous effects of HPV oncogenes, expressed only in the cervical epithelia, on the stroma, thus defining new roles of the tumor microenvironment in cervical carcinogenesis;
- defined the recently identified mouse papillomavirus, MmuPV1, to be a highly informative model for high-risk cutaneous HPVs in causing skin disease and cancer, at the pathophysiological, molecular and genomic levels;
- developed high-resolution imaging strategies to view multiple steps in replication of the HBV genome;
- used new imaging capabilities to discover the novel association of HBV reverse transcriptase (Pol) with mitochondria, identifying a potentially novel role of Pol in virus-host interactions;
- used “visible” EBV, created by this program project grant, to discover that EBV remarkably reorganizes the architecture of the host nucleus to allow it to support the amplification of the EBV genome upon lytic activation; and
- developed “visible” KSHV and discovered that it replicates during latency differently than does the highly related EBV.
“Another important feature is that our team’s interactions go beyond the program project grant’s boundaries, impacting research across the country and the globe,” says Lambert. “More than half of our publications involve collaborations outside the grant.”
He adds, “By having investigators work on shared projects focused on one or more human tumor viruses, we aim to use advances in understanding one virus to foster experiments on others. These collaborations are aided by meetings at which faculty discuss findings, technical problems, breakthroughs and much more.”
More than a quarter of the team’s studies in the past five years involved two or more program project grant labs. For instance, Lambert — who has developed powerful mouse models to understand oncogenesis by the human papillomavirus HPV16 — works with Ahlquist to build on their findings that the tumor microenvironment plays critical roles in cervical carcinogenesis. And Loeb is working with Ahlquist and Sherer to define the replication steps of human HBV using high-resolution and live-cell imaging technologies that are shared with Johannsen and Sugden.
In other collaborative work, Mertz and Kenney’s laboratories focus on understanding the regulation of EBV’s switch from latent to lytic (replicating) states with the goal of developing beneficial therapies.
“We want to better understand what controls that switch by looking at cellular factors in strains of EBV. We then look for drugs — lytic-induction therapy — that can switch the virus from its dormant state into its replicating state, which it must be in for drugs to work. After we test drugs in a petri dish, we progress to testing the successful compounds in mouse models to see whether they effectively kill cancer cells without harming normal cells,” explains Mertz.
Kenney describes a recently published study in which the team found that a specific base pair change present in certain cancer-associated EBV strains has a large effect on the activity of a critical EBV gene promoter.
“This viral promoter, which drives the switch from latent to lytic infection, is more active in the cancer-associated EBV strains, making them able to produce lots of infectious virus,” she says. “We believe that the importance of this promoter alteration is that it allows the virus to reproduce more actively, particularly when patients are co-infected with malaria.”
Kenney says the presence of malaria is why EBV-positive Burkitt’s lymphoma appears primarily in the “malaria belt” in Africa but is uncommon in the United States. Researchers believe malaria infection is a co-factor in causing cancer in Africa, and she predicts other co-factors that preferentially activate the cancer-associated promoter variant could be responsible for southern China’s high incidence of NPC.
“Although almost everybody is infected with EBV, researchers don’t fully understand why it causes cancer in only a small percentage of people, nor why it causes different cancers regionally,” says Kenney.
Johannsen notes, “Immunocompetent people require more cellular mutations to develop EBV-associated tumors. Contracting EBV is one step in a multi-step process to get cancer, but what are the other steps? Our work aims to answer questions like this.”
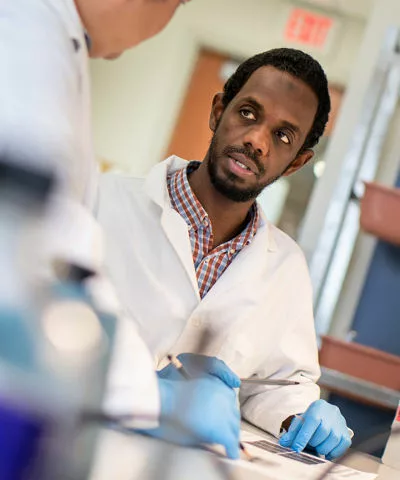
In addition to investigative work, Carbone Cancer Center faculty members share their knowledge with the next generation of researchers through a grant-funded Virology Training Program, led by Lambert. Aimed at predoctoral and postdoctoral trainees interested in all aspects of virology, it has 19 faculty members, including all program project grant team members, who study a broad variety of viruses, including those that infect plants and insects, and others that cause human cancers. Also, some study viruses related to emerging diseases, such as Ebola and new strains of influenza.
Through research and teaching, McArdle Laboratory’s faculty members continually search for and share innovative discoveries and approaches in their quest to understand viruses, prevent illnesses and develop treatments for patients here and throughout the world.