Perspectives: Cellular Pharmaceuticals Meet the Wisconsin Idea
Jacques Galipeau explains how the advent of cellular therapy has lifted restraints by using living cells as drugs.
Ask nearly anyone at the University of Wisconsin Carbone Cancer Center about its director, Howard Bailey, MD (PG ’91), and you likely will hear about his good ol’ midwestern modesty. A North Dakota native, Bailey was raised and educated in his home state through medical school prior to his residency in Michigan and eventual move to Wisconsin for post-graduate work.
He has not forgotten his roots, even as he has risen to lead one of the top cancer research centers in the United States. He prefers to shine the spotlight on others rather than having accolades directed toward him.
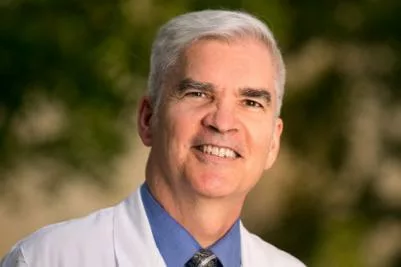
However, when you talk to Bailey about UW Carbone as an institution, he can’t conceal his pride. It is Wisconsin’s only National Cancer Institute (NCI)-designated comprehensive cancer center. Nationwide, only six cancer centers — including UW Carbone — can claim the high honor of being among the first group, in 1973, to receive that designation by the NCI. And, while few of these centers have had Nobel Prizewinning work conducted at their institutions, UW Carbone is proud that Howard M. Temin, PhD, received the Nobel Prize in Physiology or Medicine in 1975, along with two researchers from other universities.
Bailey, who became UW Carbone’s director in 2015 after serving on its faculty and as the interim director, is well prepared for his role. He recognizes the center’s strengths from before his tenure as director, and he gives credit where credit is due. He draws upon strengths to elevate UW Carbone in its national prominence, including acceptance into elite networks. And, in 2017, during UW Carbone’s five-year “checkup” required by the NCI to continue as a comprehensive cancer center, Bailey led the program to its largest rating increase to date.
Specifically, the center passed its re-application renewal with flying colors, retaining its status as Wisconsin’s only NCI-designated comprehensive cancer center and extending a $5 million per year grant for core funding over the next five years.
About the first such renewal process under Bailey’s leadership, he characteristically downplays his role in the successful score and states, “Many people worked long and hard to achieve it.”
UW School of Medicine and Public Health Dean Robert N. Golden, MD, notes, “Under Dr. Bailey’s leadership, UW Carbone has dramatically accelerated its progression to national prominence. The rigorous peer-review process confirmed the center’s growing recognition as a rising star in the very selective galaxy of NCI-designated comprehensive cancer centers.”
With pride, Bailey shares, “We strongly believe in the value of what we do and what we bring to our patients, to our communities and to Wisconsin. It’s always helpful to have established leaders from other well-known cancer centers review us and give their unbiased view of what we are accomplishing.”
He continues, “We were unanimously voted as ‘outstanding.’ Only a few centers in the nation receive that score or better.”
In general, Bailey believes UW Carbone always has had the potential for this rating. “We consistently have had great faculty researchers and staff,” he says. “What we’ve done is get them more involved by having them determine what the Carbone Cancer Center is and help run it.”
With nods to the past and boosted by recent success, Bailey is leading UW Carbone to even loftier goals: increasing patients’ access to groundbreaking clinical trials; fostering stronger connections with communities in addition to Madison to improve health outcomes throughout Wisconsin and beyond; and advancing research in strategic areas, such as cancer biomarkers, imaging and immunotherapy.
Prior to Bailey coming to the School of Medicine and Public Health and UW Carbone for a medical oncology fellowship and research fellowship, respectively, and joining the school’s faculty in 1994, cancer research at UW–Madison was already making a name for itself. In 1940, Harold Rusch, MD ’33, formed the McArdle Laboratory for Cancer Research and established the nation’s first cancer research department, the School of Medicine and Public Health Department of Oncology.
Rusch served as McArdle’s inaugural director until 1972, when he turned his attention to developing the UW Clinical Cancer Center, which subsequently was renamed the UW Comprehensive Cancer Center and, in 2006, the UW Carbone Cancer Center to honor its second director, Paul P. Carbone, MD.
“After President Richard Nixon announced the National Cancer Act of 1971, Dr. Rusch was appointed to the president’s national cancer panel,” recalls Bailey, who is the Andy and Susan North Professor of Cancer Research. “The panel convinced President Nixon that the government needed to put more money into cancer research, and one of the things they convinced him of was making these comprehensive cancer centers.”

UW Carbone’s focus on clinical research and treatments complements McArdle’s laboratory research. Over the decades, physician-scientists at UW–Madison have collaborated on numerous groundbreaking oncology-related investigations and made huge strides in patients’ health outcomes.
In the 1960s, for example, UW Professor Fritz Bach, MD, was a pioneer in bone marrow transplantation, a technique still used today to treat a variety of diseases, from cancer to immunodeficiency syndromes. Paul Sondel, MD, PhD ’75 (PG ’80) — now a professor and research director of the Division of Pediatric Hematology, Oncology and Bone Marrow Transplant in the School of Medicine and Public Health Department of Pediatrics — recalls how working in Bach’s lab as an undergraduate propelled him into his physician-scientist career working on neuroblastoma immunotherapy.
“At that time, a lot was being written about early mouse experiments from a variety of labs, indicating that the same immune system that could reject an organ transplant might be able to be trained to reject cancer,” says Sondel, who has dedicated his four-decade research and patient care career in this field at UW Carbone and the American Family Children’s Hospital. “When President Nixon declared the War on Cancer, it was clear to me that I should delve into analyzing whether the immune system could recognize cancers.”
Fast forward to the 2000s, and Sondel’s work has resulted in a U.S. Food and Drug Administration-approved immunotherapy for relapsed or refractory pediatric neuroblastoma. The therapy increases survival rates from 25 to 50 percent.
“We are pleased that this immunotherapy regimen has become the standard of care in the United States for children with high-risk neuroblastoma,” exclaims Sondel. “We are investigating the use of personalized medicine to identify individuals with certain genes that might make them most likely to benefit from this treatment.”
Another UW–Madison researcher, V. Craig Jordan, PhD, began pioneering treatments for estrogen receptor-positive breast cancers long before Bailey’s time as UW Carbone director. Now a professor at the MD Anderson Cancer Center in Houston, Jordan created a strong foundation for current physician-scientists’ work at UW–Madison.
Among them is Ruth O’Regan, MD, chief of the Division of Hematology, Oncology and Palliative Care in the School of Medicine and Public Health Department of Medicine and associate director of clinical research at UW Carbone, who worked with Jordan at Northwestern University.
“Earlier in my career, I was involved in studying resistance to endocrine therapy in breast cancer,” she says. “At UW–Madison in the 1990s, Dr. Jordan was responsible for developing tamoxifen as a breast cancer drug,” recalls O’Regan, whose internationally recognized research aims to continue identifying mechanisms of resistance to breast cancer therapies and developing innovative treatments.
As cancer research has progressed throughout the United States, UW Carbone remains one of 70 NCI-designated cancer centers, but it does not rest on its reputation as one of the originals. Case in point, in 2016, UW Carbone was accepted into the elite National Comprehensive Cancer Network, a not-for-profit alliance of 28 of the world’s leading cancer centers; that network writes the standards for cancer care nationally and, increasingly, globally.
In preparation for the 2017 NCI review, when leaders from that agency and other NCI-designated cancer centers evaluated dozens of aspects of UW Carbone, Bailey and colleagues paid particular attention to reviewers’ areas of focus: the amount of external funding the center receives, the impact of its research and the number of patients who benefit through clinical trials.
Results show many measures of success, including UW Carbone’s robust partnerships with local philanthropists — including the Andy North and Friends golf and trivia events and the Garding Against Cancer events — which have boosted fundraising. These efforts help fund early-stage, high-risk research, which increases researchers’ success in obtaining federal grants.
Further, since Bailey became director, the number of patients enrolled in clinical trials at UW Carbone has doubled. This corrected a local and national trend of declining clinical trial enrollment for the prior five to 10 years.
Looking into reasons for the local trend, the center’s leaders discovered that each disease group had been run like an individual small business, meaning that each group was responsible for writing all study protocols, obtaining human subjects approval, negotiating budgets with industry sponsors and caring for patients in their trials, according to Sarah Stewart, assistant director of clinical research at UW Carbone.
“Because patient care takes priority, under the old model, getting a new study up and running would sometimes be put on hold,” she explains. “Industry partners prefer sites that can open trials quickly and produce results, and we were not always getting access for patients to trials we would have liked to open.”
Bailey and Peter Connor, UW Carbone associate director of administration, worked with clinical research teams to determine how best to meet needs and accomplish goals more efficiently than in the past.
“We encouraged clinical researchers and gave them autonomy to make the necessary changes,” says Connor, adding that successful results led to centralizing all aspects of clinical research.
Today, disease-specific research teams focus on enrolling and caring for patients on trials, while a fiscal team works on all budgets, a regulatory team obtains human subjects approvals, and dedicated coordinators propel studies through other steps of activation. Enrollment is the highest since 2009 and just over the 2012 level.
“Dr. Bailey deserves all the credit,” Stewart states. “The reason our accrual is increasing and our time-to-trial activations are decreasing — important metrics that mean we’re getting patients on study as quickly as possible — are due to the centralized structure he created.”
Beyond this, Bailey points to other improvements that were underway before he became director that helped buoy the center’s success. An example is the construction of the Wisconsin Institutes for Medical Research, an innovative complex that brought together several cancer-focused groups — among them the Department of Human Oncology, McArdle Laboratory and the Department of Medicine’s Division of Hematology and Oncology. This collaborative hub on the west end of UW–Madison is attached to the Health Sciences Learning Center — home to the School of Medicine and Public Health — and the Clinical Science Center, which houses UW Hospital and UW Carbone.
While celebrating the successful core grant renewal, Bailey, Connor and other colleagues are taking steps to further elevate the center’s reputation. They have structured the UW Carbone Strategic Plan around four key initiatives:
Imaging and biomarker research have been identified as priority research areas. Bailey cites a collaboration among Zachary Morris, MD, PhD (PG ’16), assistant professor, Department of Human Oncology, and Jamey Weichert, PhD, professor, Department of Radiology, and Sondel as being particularly strong in these areas.

With a $2.5 million NIH Cancer Moonshot Grant, they are developing an approach to immunotherapy that uses a novel form of molecular targeted radionuclide therapy (MTRT) to enhance the effectiveness of immune checkpoint inhibitors to treat metastatic cancer. The therapy, which was developed by Weichert, is administered intravenously and selectively taken up by tumors, which receive a low dose of radiation. Rather than killing the cancer cells, this low dose of radiation temporarily eradicates suppressive lymphocytes in the irradiated sites to help restore the immune system’s ability to recognize and kill cancer cells. The radiation also increases tumor cells’ susceptibility to the immune response.
“The real key is that MTRT allows us to effectively deliver radiation to all tumor sites—even ones we can’t see,” Morris says. “We cannot achieve that short of doing total body radiation with external beam treatments. But that would deplete lymphocytes everywhere and prevent any immune response. In this research we’re depleting some immune cells temporarily at the radiated tumor sites. The therapy does not radiate the lymph nodes, spleen or bone marrow, so there’s a huge reservoir we can draw on to regenerate an effective anti-tumor immune response.”
Morris’ group and the other nine research teams receiving this grant nationwide are inaugural members of the NIH’s Immuno- Oncology Translational Network, which aims to facilitate collaboration and spur further progress in the fight against cancer. “I think working with these other researchers could be one of the most impactful aspects of this award,” says Morris. “I also believe, in the future, we’ll be able to translate this treatment to patients with essentially any cancer.”
Bailey observes, “UW Carbone fosters this type of innovative collaboration with strong potential for clinical relevance.”
He points with equal pride to a shining example of UW Carbone’s outreach efforts: the Precision Medicine Molecular Tumor Board, a statewide service available to oncologists throughout Wisconsin. Working in partnership with the UW Collaborative Genomics Core and UW Carbone, the Tumor Board calls upon UW–Madison experts in pathology, genomics, genetic counseling, medical oncology and pharmacy, as well as collaborators from health systems throughout the state. The board focuses on helping patients who do not have a curable treatment option. Those involved discuss and analyze tumor genotypes and molecular abnormalities to recommend specific targeted therapies.
According to the board’s co-leaders — Mark Burkard, MD, PhD, and Dustin Deming, MD ’07 (PG ’10, ’12), associate professors, Department of Medicine, Division of Hematology and Medical Oncology — cancers traditionally have been classified by their site of origin, meaning breast cancer starts in the breast, and colon cancer starts in the colon. This paradigm is now being challenged through the Tumor Board.
“Since 2015, we have led a bimonthly, web-conferenced statewide tumor board through which physicians can discuss cancer patients, including their tumor DNA test results. To date, the Tumor Board has reviewed DNA testing and provided specific recommendations for more than 1,000 patients,” says Burkard.
Deming, who also holds an appointment in the Department of Human Oncology, adds, “Through the Tumor Board’s work, every cancer patient in Wisconsin can have access to the most sophisticated, state-of-the-art approach to personalized oncology care.”
Reflecting on all of UW Carbone’s past success and thinking broadly about its future, Bailey concludes, “We have a responsibility to impact cancer care and research throughout Wisconsin and beyond; we are proud to be among the long line of UW–Madison faculty and staff who incorporate the Wisconsin Idea into everything we do.”