Wisconsin’s Mary Lasker a Driving Force Behind National Cancer Act
Lasker is widely credited as one of the driving forces behind the National Cancer Act.
In his 1971 State of the Union address — just over 50 years ago — President Richard Nixon called for an unprecedented national approach to fighting one of our country’s greatest enemies: cancer.
“The time has come in America when the same kind of concentrated effort that split the atom and took man to the moon should be turned toward conquering this dread disease,” the 37th U.S. president announced. “Let us make a total national commitment to achieve this goal.”
Less than a year later, on Dec. 23, 1971, Nixon signed the National Cancer Act into law. The landmark piece of legislation would fundamentally reshape the cancer research landscape in America, provide new funding opportunities, and officially kick off what’s now known as the “war on cancer.”
To assist in that fight, the National Cancer Act called for the creation of cancer centers throughout the United States for clinical research, training and demonstration of advanced diagnostic and treatment methods relating to cancer. These would become known as comprehensive cancer centers, and the University of Wisconsin–Madison — an institution already on the cutting edge of cancer research, drawing on decades of research by investigators such as Elizabeth C. Miller, PhD, and Harold Rusch, MD ’33 — saw an opportunity.
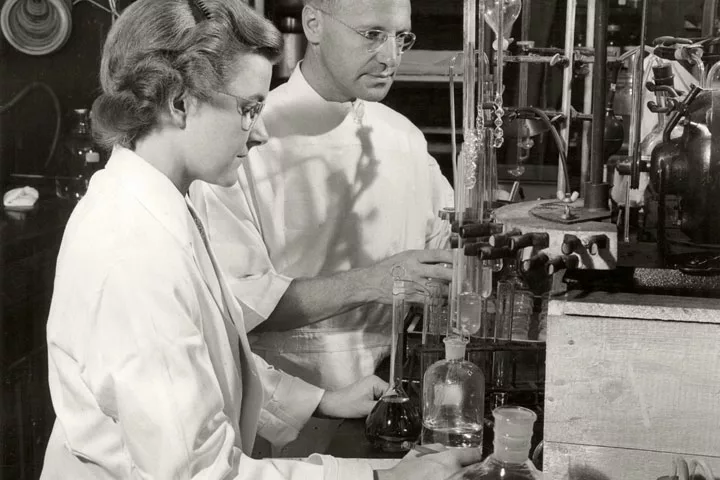
Under Rusch’s leadership, UW–Madison submitted a proposal to the National Cancer Institute (NCI) to create a comprehensive cancer center. This led to the creation in 1972 of the UW Clinical Cancer Center, which was awarded comprehensive status a year later by the NCI. At the time, only five other institutions received the NCI’s first “comprehensive” designation — an honor that UW–Madison has maintained ever since.
With the infrastructure taking shape across the United States to fight cancer, the challenge then became: what next? It was uncharted territory, but the newly designated UW Comprehensive Cancer Center played an outsized role in charting a course.
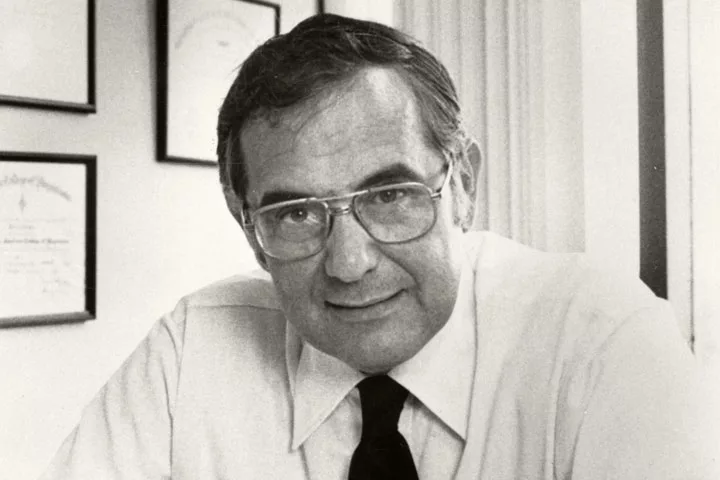
“UW–Madison researchers were heavily involved in not just the genesis of cancer research, but they were heavily involved in advising the federal government in the early 1970s on what the war on cancer should be,” says Howard Bailey, MD, director of the UW Carbone Cancer Center — the center’s new name as of 2006, in honor of Paul P. Carbone, MD, who served as the center’s director for nearly 20 years.
Bailey continues, “Our people were able to help shape policy based on what they knew was important and had been studying for decades.”
In the 1930s, Frederic E. Mohs, MD ’34, a surgeon at UW Hospital and Clinics (now UW Health) and faculty member at the UW Medical School (now the UW School of Medicine and Public Health), developed a procedure — Mohs surgery — to treat patients with skin cancer. Mohs rose to the level of emeritus clinical professor of surgery.
In the 1940s, the McArdle Memorial Laboratory for Cancer Research opened its doors and became the first cancer research center founded by a university in the United States.
In the 1950s, Charles Heidelberger, PhD, SMPH professor of oncology, developed fluorouracil, also known as 5-FU, which would eventually become one of the most widely used chemotherapy drugs in the world.
And in the 1960s, Fritz Bach, MD, a physician-scientist and SMPH professor, developed a compatibility test between tissue donors and recipients, which enabled him to lead one of the world’s first successful matched bone marrow transplants in 1968.
When it came to researching and treating cancer, UW–Madison was clearly ahead of the curve.
“There was this collection of forward-thinking researchers here who decided that having some specific plans for dealing with cancer was important,” Bailey states. “The University of Wisconsin has always been on the forefront of wanting to study the maladies that were important to its state residents, and clearly they recognized that cancer was a priority.”

But even with decades of experience, the ambitious goal that President Nixon laid out in 1971 — to cure cancer — would not be easy.
Richard Burgess, PhD, SMPH emeritus professor of oncology, likens fighting cancer to standing next to a railroad track and being asked to stop an oncoming train with nothing but a wrench in your hand.
“There’s no way you’re stopping it,” he says. “You could throw that wrench at that train a million times and never even come close to stopping it. That’s the way our knowledge was back then.”
But Burgess notes that if you studied the diagrams and the inner workings of the train, you could potentially build a foundation of basic knowledge necessary to achieve the goal.
“You could recognize that there are certain vulnerable spots in the train where, if you stuck a wrench in where the gears are coming together, you could stop the train,” he describes. “And that’s exactly what’s happened over the last 50 years.”
In 1971, Burgess had just arrived in Madison to work in the McArdle Laboratory. Funding from the National Cancer Act helped him establish his lab and dive into research. Having discovered the first positive transcription factor — a protein that effectively turns genes “on” — Burgess gradually built a research operation dedicated to understanding the ins and outs of the protein machinery of gene regulation, which helped researchers build their knowledge of what cancer is and how it operates.
As Burgess likes to say: “Today’s basic research produces tomorrow’s new treatments.”
Throughout the years, research advances made at UW–Madison have directly led to new, more effective treatments for cancer. That includes tamoxifen, which became one of the most widely utilized treatments for both preventing and treating breast cancer.
UW–Madison also is the home of TomoTherapy, a specialized form of radiation therapy that targets cancer cells and avoids healthy cells.
Today, that legacy of developing paradigm-shifting cancer therapies continues in new and exciting ways, from creating personalized vaccines made from a patient’s own cells to developing more targeted and effective immunotherapies that can be used as first-line treatments.
For instance, the Program for Advanced Cell Therapy was launched in 2016 to develop personalized cell technologies for improving health outcomes in children and adults with unmet medical needs, such as radiation-caused dry mouth, and testing those therapies through first-in-human clinical trials.
UW Carbone also has established itself as a leader in precision medicine; it is home to the Precision Medicine Molecular Tumor Board (PMMTB). Developed as a collaboration among UW Carbone and some of the state’s largest oncology practices, the board reviews cancer cases based on patients’ specific genetic mutations, and it recommends patient-specific targeted therapies.
Since its inception six years ago, the Tumor Board has reviewed more than 5,500 cases, with the annual number of cases increasing every year.
“We learn a lot from our patients, and it inspires us to try and understand what’s going on with individuals or groups of patients who have unusual cases,” shares PMMTB co-director Mark Burkard, MD, PhD, SMPH professor of medicine. “But at the end of the day, I think the biggest win is for the patients.”
A lot has changed over the past 50 years. There are now more than 50 NCI-designated comprehensive cancer centers in the United States. Thanks to significant research advances made possible by the National Cancer Act of 1971, cancer is much more preventable and treatable. And more cancer patients survive today than ever before.
What hasn’t changed during all this time is UW Carbone’s spirit of innovation, a deep commitment to research and patient care, and a desire to make life better for individuals with cancer.
It’s what the UW Carbone Cancer Center’s namesake would have wanted because it’s what he preached. After all, he had a favorite phrase, one that the center still lives by today: “Cancer research has a face: the face of our patients.”