Rolf Lulloff’s Lifelong Passions Fuel Today’s Ventures
After losing his wife to Parkinson's, Lulloff co-founded an organization that provides education and support for people and families affected by neurological conditions.
As a child in the Republic of Guinea, West Africa, Kaïssa Sylla always knew she wanted to be a doctor. She moved to the United States for college when she was 18 and lived with her older siblings. Sylla graduated with a bachelor’s degree from the University of Delaware in spring 2015 and got married that summer. She intended to apply to medical school right away, but an extraordinary series of events deferred her plans.
Ten days after celebrating Sylla’s wedding in Guinea, her mother passed away, and two months later, in Delaware, Sylla had a stroke. She was hospitalized for 10 days and doubted she would have the stamina for medical school, so she decided to focus on starting a family; she now has a daughter and a son.
Although she was incredibly busy, Sylla still dreamed of becoming a physician, so she tested her readiness to withstand the rigors of medical school by attending graduate school. As she earned a master’s degree in medical sciences from the University of Vermont, she got her confidence back and started applying to medical schools, including the University of Wisconsin School of Medicine and Public Health.

She feels like she received “a sign” related to a profound date. On February 21, 2018, her father had passed away in Guinea. On that date in 2021, she received a call from a School of Medicine and Public Health admissions officer telling her she had been accepted to the school.
“My last few conversations with my dad were about not abandoning my dreams to go to medical school! The call totally took my sadness away,” says Sylla, who now is a second-year medical student at UW and is considering neurosurgery as one of her options for a career.
The tragic circumstances surrounding her parents’ deaths gave Sylla clarity about the kind of physician she wants to be and fuel her passion to do all she can to improve medical care for the Guinean people.
She had watched her mother suffer and decline because there was no oxygen available at the hospital. Despite Sylla’s valiant efforts to seek help, she recalls staff appearing apathetic during her mom’s medical crisis.
“That traumatic experience marked me the most. I thought, ‘This is not right,’ and it defined the type of doctor I want to be,” she says. “Experiencing the way the doctors and nurses were so attentive and listened to me after I had a stroke was so different from my mom’s experience. It redefined my motivation to go to medical school and my end goal, which includes working in medical education.”
Medical system limitations and power outages in Guinea’s capital city, Conakry, also played a role in her father’s death because his much-needed oxygen required electricity. Being in the United States at the time left Sylla feeling helpless, but the COVID-19 pandemic provided her first opportunity to see how she might support the Guinean community.
Sylla connected online with several doctors and nurse practitioners from Guinea who practice in the United States. Via radio and online platforms, she and these health care providers shared U.S. Centers for Disease Control and Prevention (CDC) recommendations to French-speaking Guinean people living in the United States. The team also raised money to send materials to Guinea to support care for COVID-19 patients in the country’s only intensive care unit (ICU), which has 14 beds.
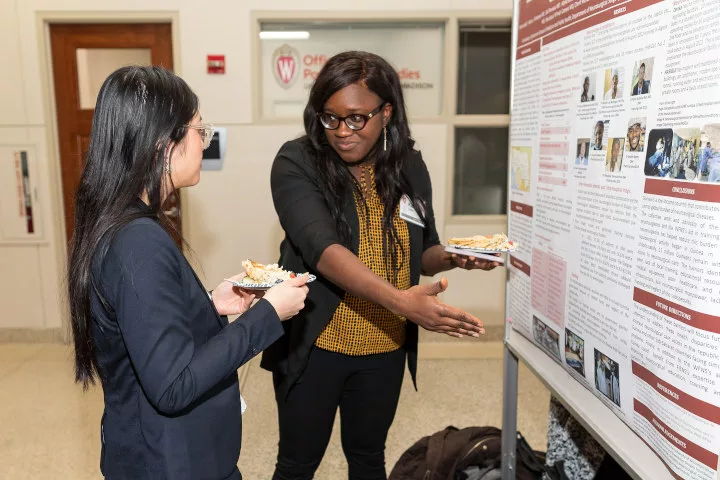
The summer before medical school, Sylla visited Guinea to shadow a neurosurgeon she met through the COVID-19 volunteer group. The next year, she returned to Guinea as a scholar in the School of Medicine and Public Health’s Shapiro Summer Research Program, through which the school’s medical students can participate in full-time summer research projects under the mentorship of faculty members.
Sylla’s abstract, “Guinea: Barriers to Achieve a Comprehensive National Neurosurgical Care Delivery System in a Sub-Saharan Country,” outlines some of the medical system’s challenges. For instance, in Guinea, neuro-trauma from motor vehicle and motorcycle accidents is the second major cause of disability in young males. However, the country has only seven practicing neurosurgeons, one magnetic resonance imaging scanner and two computed tomography scanners, so neurosurgical interventions can be performed on less than 10 percent of reported accidents. The nation also has no neurosurgical training program, and intern doctors wait up to 10 years post-graduation to obtain a scholarship for training abroad.
Sylla was impressed with Guinean neurosurgeons whose sophisticated technical skills and knowledge of anatomy compensate for the lack of equipment. She was especially inspired by the interns who work without pay.
“Even though you’re not getting formally trained in neurosurgery, you still wake up every day and go to the hospital because you hope to make someone feel better, and you want to learn. That was amazing to me, that’s dedication,” she reflects.
Sylla’s mentor from the School of Medicine and Public Health, Robert Dempsey, MD, the Manucher J. Javid Professor and Chair, Department of Neurological Surgery, says, “This study carefully defines the resources available, but more importantly, brings together the personnel necessary to design a national neurosurgical care delivery system. Such research is the basis of education-based improvements in health care in low- and middle-income countries, giving us the greatest hope for future improvement.”