Head and Neck SPORE Grant
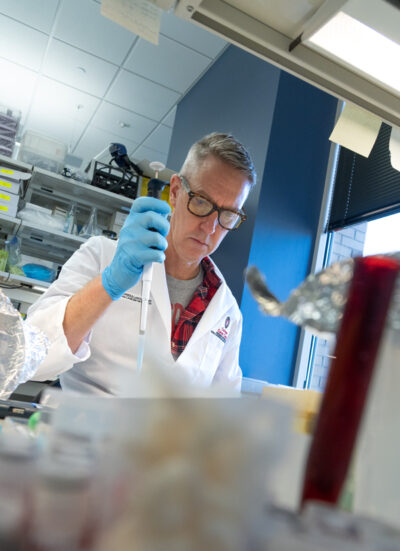
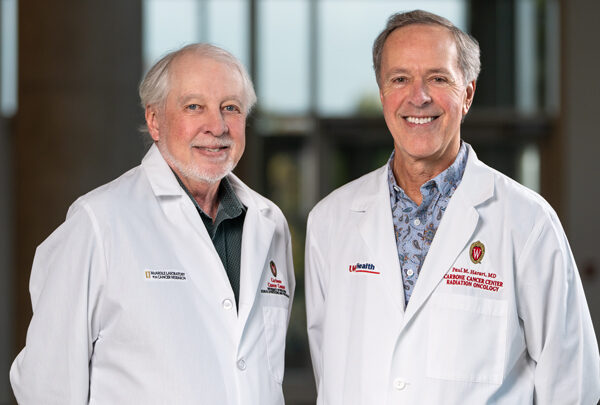
Harari and Paul F. Lambert, PhD ’85 (basic science co-leader), direct the head and neck SPORE grant. Lambert is the director of McArdle Laboratory for Cancer Research and chair of the Department of Oncology. Approximately 35 faculty members and 120 staff members are involved in the head and neck SPORE grant, which includes these scientific projects:
Project 1: Targeted Radionuclide Therapy
Leaders: Zach Morris, MD, PhD (PG ’16); Jamey Weichert, PhD; Paul Harari, MD
Researchers are testing a targeted form of radiation therapy (NM600) that, ideally, will result in greater patient survival. The project combines the most common form of immunotherapy with NM600, which is given via injection. One of the excellent features of this type of radionuclides is they can be given diagnostically and therapeutically, meaning they can both image and treat tumors.
“We call it a theranostic agent,” Morris says. “With the help of PET [positron emission tomography] scans, we first determine whether the patient’s tumor will absorb the agent before we inject a therapeutic dose. This process lets us create a personalized prescription to deliver the desired amount of radiation for each patient.”
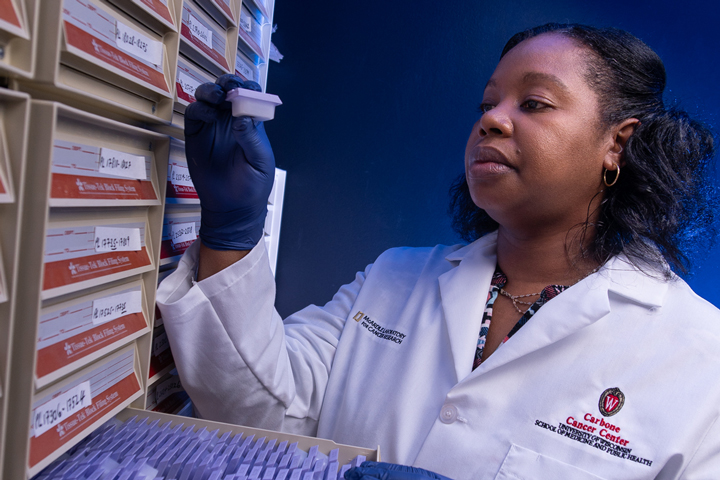
Project 2: Biomarker Prediction of Treatment Outcomes
Leaders: David Beebe, PhD ’94; Paul Harari, MD
Health care professionals need better tools to predict whether a treatment will increase survival for head and neck cancer patients. This project advances a powerful, patient-specific bioengineered model — developed at UW–Madison — built from individual patient tumor cells to predict tumor response and investigate biomarkers of response in tumor tissue. A clinical study will be performed to test the feasibility of using response data from the model to guide head and neck cancer treatments for individual patients based on specific tumor characteristics. This project combines patient-specific data, such as single-cell RNA sequencing, to identify patterns that predict how well treatments work. The result will improve decision‑making.
Project 3: Protein-Blocker to Enhance the Body’s Immune System
Leaders: Deric Wheeler, PhD ’04; Justine Yang Bruce, MD
Researchers hope to show that a new drug can block the unwanted impact of two proteins found on tumor cells — Axl and MerTK. When these proteins work in tandem, they prevent the immune system from fighting cancer in patients who have been given immunotherapy. Mouse model research demonstrates that reprogramming the microenvironment that feeds a tumor in a way that reignites the immune system results in a more powerful anti-cancer response. If similar results are found in humans, immunotherapy could more effectively treat patients with specific head and neck cancers.
Prostate SPORE Grant
Jarrard and Douglas McNeel, MD, PhD (co-PI), professor, Department of Medicine, and genitourinary oncologist, UW Health, are overseeing UW Carbone’s prostate SPORE work, in which more than 50 faculty and staff members are contributing. This grant is supporting numerous developmental ideas and three main research projects:
Project 1: Enhancing Understanding of How Prostate Cancer Spreads
Leaders: Joshua Lang, MD (PG ’08, ’11); Sheena Kerr, PhD; Melissa Skala, PhD; David Jarrard, MD
Researchers know that prostate cancer cells do not act alone; they can “trick” nearby cells in the microenvironment that helps feed the cancer. This makes blood and lymph vessels “leakier,” giving cancer cells a new pathway to the rest of the body. This project recreates a patient’s tumor and its microenvironment on a chip, allowing researchers to examine how genetic and cellular changes cause the cancer to spread. A better understanding of which cancers are most lethal would position researchers to test treatments that could prevent metastasis.
“There are many new therapies being developed that target these other cell types in the tumor environment. We are studying how and for whom these therapies will be most effective,” says Lang.
Project 2: An Anti-cancer Vaccine to Prevent Metastasis in High-Risk Patients
Leaders: Douglas McNeel, MD, PhD; Christos Kyriakopoulos, MD; David Jarrard, MD
For more than 20 years, UW–Madison researchers have been working to develop a DNA vaccine that, when given in conjunction with testosterone-reducing hormone therapy and immunotherapy, makes cancer cells more “visible” to the body’s immune system. Because hormone therapy causes cancer cells to over-express their androgen-receptor protein, the vaccine appears to more easily recognize that protein, signaling the immunotherapy treatment to kill more cancer cells. Early clinical trials have shown that high-risk patients who received the vaccine are living longer than unvaccinated individuals; however large-scale, Phase III trials are still to come.
“If we can clearly demonstrate that our vaccine is triggering cancer-destroying, tumor-specific immune responses, we could see transformative increases in survival times,” says McNeel.
One of the prostate SPORE team’s external advisors, Howard Soule, PhD, executive vice president and chief science officer of the Prostate Cancer Foundation, says this vaccine project could be a tremendous breakthrough.
“Having a project included in the SPORE grant typically means that the NCI thinks you are on to something,” says Soule. “Other cancer vaccines have been tried, but what makes this unique is that it is targeted to the central activity that leads to progression and death. Once tested on a larger scale, this vaccine could be off to the races.”
Project 3: Using Lesion-Response Technology to Treat Patients with Greater Precision
Leaders: Glenn Liu, MD (PG ’00, ’02); Robert Jeraj, PhD; John Floberg, MD ’14, MS ’10, PhD ’12
This project seeks to extend survival time for patients with advanced prostate cancer — namely cancer that has already spread elsewhere and no longer responds to testosterone-reducing hormone therapy. UW–Madison researchers believe that even though these patients’ conditions are not curable, conventional clinical decision-making is too dichotomic; the patient is classified as either “responding” or “progressing.”
By examining how each lesion — not just a subset — responds to treatment, physicians can make decisions about care that improve patient outcomes.
“Our work shows that patient outcome is driven by resistant lesions,” Liu says. “Identifying and targeting that resistance with lesion-tracking software can improve patient care by optimizing benefit from existing therapy options.”
A Patient’s Perspective
SPORE-recipient institutions must include patient advocates on their teams. In this capacity, Marshall Flax is among those who advise the head and neck SPORE team; others similarly advise the prostate SPORE team.
When he was diagnosed with stage 4 tonsil cancer in 2003, Flax was treated with radiation and chemotherapy that saved his life but left him susceptible to swallowing problems. He says having patient advocates on SPORE teams helps remind researchers that their work has a real-world impact on people’s lives.
“When they start talking about something like dry mouth, that is when we pipe up and keep them focused on the side effects that may come with life-saving treatment. It is wonderful to know that this research may help future patients avoid things like dry mouth or swallowing difficulties.”