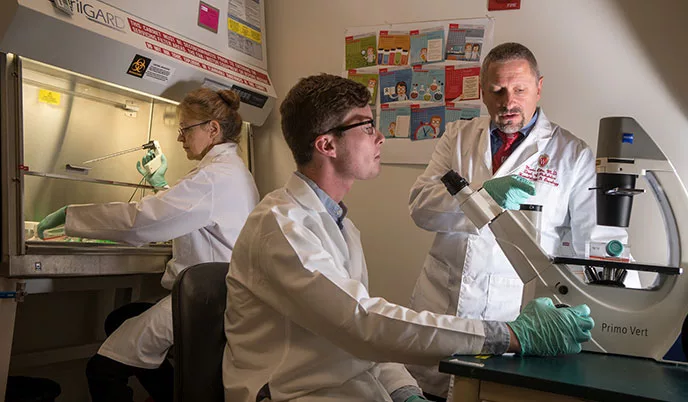
In separate work that lays the foundation for simpler, more cost-effective immunotherapy, Douglas McNeel, MD, PhD, professor, Department of Medicine, and director, Solid Tumor Immunology, UW Carbone Cancer Center, has been investigating T cell-activating therapies, or vaccines, as treatments for prostate cancer. The concept with this approach is generating tumor-fighting immune cells directly, without having to prepare them in the laboratory and infuse them back into patients. Over the past 15 years, McNeel and his team have conducted several clinical trials with two vaccines that are currently in testing at the Carbone Cancer Center and elsewhere in the United States.
Cellular immunotherapy has been remarkable for cancer treatment, and UW School of Medicine and Public Health experts are taking it far beyond cancer.
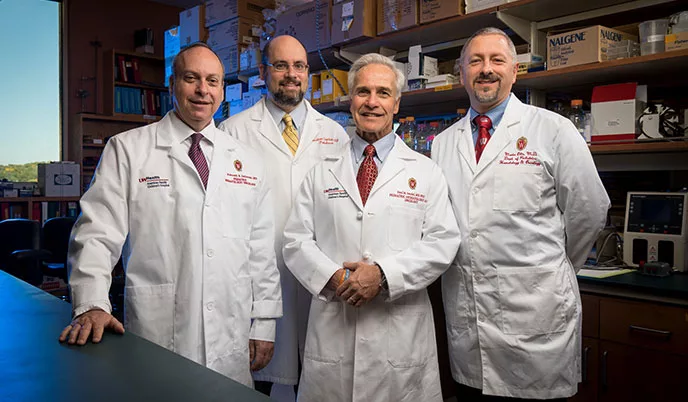
For instance, Hematti is working with Dixon Kaufman, MD, PhD, the Ray D. Owen Professor and chief, Division of Transplantation, Department of Surgery, on a novel cellular immunotherapy using donor stem cells.
“We take stem cells from a kidney donor and do a stem cell transplant after the kidney transplant,” says Hematti, adding that findings could lead toward eliminating the patients’ need for immunosuppression drugs after solid organ transplantation.
The research is rapidly moving from animal models toward human clinical trials, both supported by grants from the National Institutes of Health. Hematti and Kaufman are collaborating with scientists at Stanford University to make this treatment a reality for patients at UW Health.
Through the UW–Madison Stem Cell and Regenerative Medicine Center, Hematti also has worked for more than a decade with Amish Raval, MD, associate professor, Department of Medicine, on cardioimmunotherapy. Recently, the duo has focused on using immune cells, specifically macrophages, to repair cardiac damage in animal models, and they hope to move their research into human clinical trials soon. Whether it’s for cancer treatment, organ transplants or cardiac tissue repair, cellular immunotherapy is exploding.
“Today, immunotherapy is approved as a first-line treatment for adult patients with widespread melanoma, lung cancer and several other forms of high-risk cancers in adults and children,” says Sondel.
He predicts that within the next 10 years, treatment of nearly all cancers that are not being cured by surgery alone will integrate immunotherapy.
Sondel knows that concept will take intense teamwork over time but states that the UW School of Medicine and Public Health and UW Carbone Cancer Center have world-class reputations for research being done by outstanding faculty who collaborate internally and throughout the nation — and they are making great strides in the fight against deadly diseases.
Hematopoietic Cell Processing Capabilities Expand
A $1 million expansion of cell processing capabilities at the University of Wisconsin School of Medicine and Public Health will help the academic medical center launch the next phase of cellular immunotherapy and precision medicine. The investment will allow researchers to prepare individualized cellular treatments for patients.
“It’s really satisfying because we’re nearing the point where we can offer patients more than we ever could before,” exclaims Peiman Hematti, MD, director of the University Hospital Clinical Hematopoietic Cell Processing Laboratory (CHCPL) and a professor in the UW School of Medicine and Public Health Department of Medicine. “We’ll be able to do things like perform cell expansion, genetically modify cells, manufacture CAR-T cells and create new cellular immunotherapies.”
Jacques Galipeau, MD, the Marilyn and Don Anderson Professor of Cancer Research, Department of Medicine, and director, Advanced Cell Therapy Program, UW Carbone Cancer Center, adds, “We’re talking about taking cells from a patient’s own body and putting them in a petri dish, growing a whole crop of them, modifying them and giving them back to the patient. In this scenario, the hospital becomes an infrastructure for culturing cells, and that will make University Hospital a destination for this technology.”
“As much as I’d like to see the first products out of that lab as soon as possible, patient safety is our biggest goal, and we want to do it right,” shares Hematti.
Noting that he thinks UW–Madison is ahead of the game in cellular immunotherapy product manufacturing, Hematti says, “Collectively with all the smart people we have here, the UW School of Medicine and Public Health and University Hospital are becoming a powerful center for cellular immunotherapy. The time to act is now.”