Training in Urban Medicine and Public Health
New leadership and curriculum have bolstered the legacy of the School of Medicine and Health's specialized training program that prepares future doctors to practice in underserved urban areas.
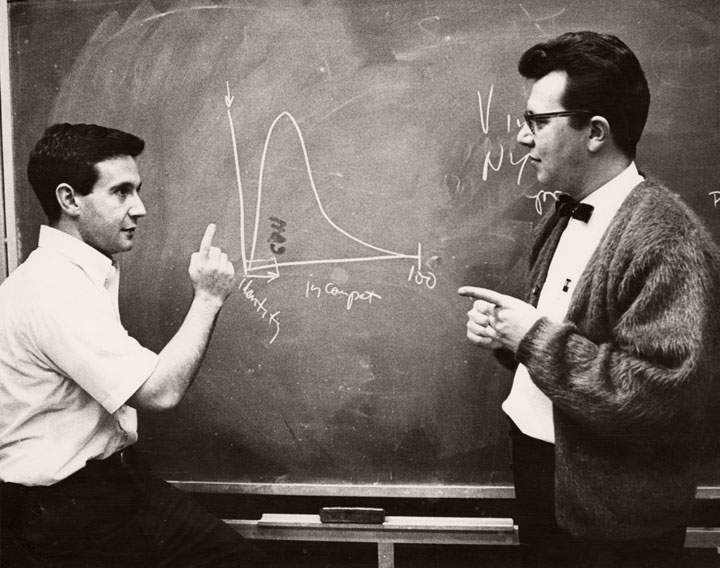
Fifty years ago, University of Wisconsin School of Medicine and Public Health Professor Fritz Bach, MD, and University of Minnesota Professor Robert Good, MD, PhD, performed the first successful bone marrow transplants, made possible by Bach’s earlier research findings.
One year later, a young, inquisitive undergraduate student — Paul Sondel, MD, PhD ’75 (PG ’80) — joined Bach’s lab and, with colleagues, has carried the torch to further the field of immunotherapy ever since.
“The national media, university and lab were still buzzing about the landmark transplants when I started working in Dr. Bach’s lab in 1969,” exclaims Sondel, now the research director of the Division of Pediatric Hematology, Oncology and Bone Marrow Transplant in the Department of Pediatrics. “I was struck by seeing news stories about it.”
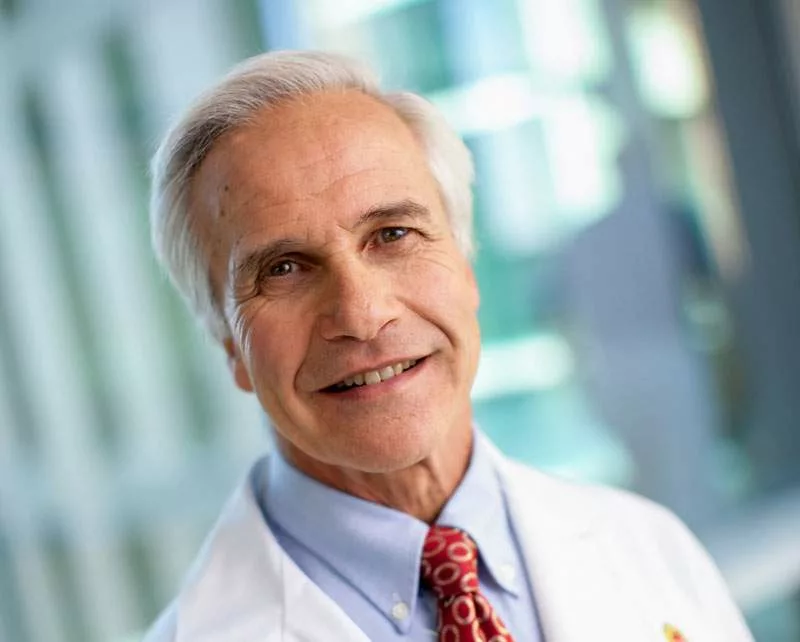
His working relationship with Bach played a huge role in Sondel’s decision to earn a doctorate in genetics at UW–Madison before he attended medical school at Harvard University, where Bach had earned his medical degree. They became lifelong friends before Bach died in August 2011 at age 77.
“I knew Dr. Bach for 42 years,” says Sondel, who did pediatric residency training at the University of Minnesota and UW Children’s Hospital in Madison (now called American Family Children’s Hospital) before he joined the faculty of the School of Medicine and Public Health Departments of Pediatrics, Human Oncology and Genetics in 1980. “He was a treasured mentor, colleague and friend.”
Bach’s first successful bone marrow transplant, performed in 1968, was on a 22-month-old boy with Wiskott-Aldrich Syndrome, an immunodeficiency disease. The patient and his family were from upstate New York, and Bach conducted the transplant at UW Children’s Hospital. The boy’s sister had donated the bone marrow, which allowed her brother to live into adulthood.
The test that opened the door to the first successful bone marrow transplants was the Mixed Leukocyte Culture (MLC) that combined white blood cells of the patient with white blood cells of related donors to find a match by serving as a surrogate marker of Human Leukocyte Antigen (HLA) gene compatibility. French researcher Jean Dausset, MD, had identified the HLA genes on chromosome 6, and Bach proved that a donor-recipient match of the HLA genes can help predict the success of a bone marrow transplant.
“Dr. Bach figured out how to do the equivalent of a bone marrow transplant in a test tube by mixing the white blood cells of the patient and the related donor. It was a way to gauge the chances of graft versus host disease (GVHD), a lethal reaction in which immune cells attack the patient’s body,” describes Sondel, adding that any two siblings who did not react to each other in the MLC would signify a match; and any two siblings have a 25 percent chance of being a match.
Bach shared the MLC testing method with Good, which enabled him to perform a successful bone marrow transplant on a different patient in Minnesota that coincided with the transplant in Wisconsin. Research papers on the two transplants were reported side-by-side in the prestigious journal The Lancet.
Richard Albertini, MD ’63, PhD ’72 (PG ’87) — a former postdoctoral research fellow with Bach and a member of the transplant team — was at the bedside of the patient when he received the first successful bone marrow transplant by Bach.
“That was the second time we had done a bone marrow transplant on the (Wisconsin) patient,” notes Albertini. “The first time, we didn’t immunosuppress his system, but for the second, we completely wiped out his system to suppress it before the transplant, thereby enabling the transplant to grow successfully.”
Albertini saw evidence of the long-term success of the boy’s second transplant when the recipient — then an active teenager — visited him several years later at the University of Vermont.
About seven years after the first successful transplants, Bach found a way to speed up the MLC test so it required only several hours rather than six days. In addition to benefitting bone marrow transplant patients, the speeded-up test also positively impacted cadaver kidney transplant recipients, because that procedure must be done within 48 hours of the donor’s death.
“Fundamentally, we still conduct this testing, but we have a refined way of doing so,” explains Mark Juckett, MD, director of the Adult Bone Marrow Transplant Program at UW Health and a professor (CHS) in the Department of Medicine’s Division of Hematology and Medical Oncology.
Today, bone marrow transplants can be done with unrelated donors. The National Marrow Donor Program, otherwise known as the “Be the Match” program, was founded in 1986 and includes approximately 10 million potential bone marrow donors. The registry allows physicians to conduct transplants on the 75 percent of patients who need a bone marrow transplant but who don’t have a family member who is a match.
“Hopefully, through research, bone marrow transplants will continue to get easier and safer for patients, or we will find other treatments that are less risky,” says Juckett, noting that Bach’s early work and successful transplants paved the way for five decades of advances, with more on the horizon.
When transplants were first performed for children and adults with leukemia, patients were treated with high doses of chemotherapy and total body radiation in an attempt to cure the disease. The transplant was given immediately after the chemotherapy and radiation in order to rescue the patient from a major side effect of this treatment — severe damage to the patient’s normal bone marrow.
It was later discovered that immune cells from the donor, transferred to the patient with the transplant, played an important role in destroying any cancer cells that were not killed by the chemotherapy and radiation, a phenomenon now known as the “graft-versus-leukemia” effect. This realization facilitated the development of many other immune-based therapies to fight cancer.
“We’re at the beginning of new types of therapies in which patients are given cells using novel techniques,” Juckett says, referring to immunotherapies that use the body’s own white blood cells to kill leukemia and other cancers without destroying normal tissue.
Sondel has pored over the concepts behind immunotherapy for five decades.
“I remember, back in 1969, talking with Fritz Bach about the strength of the immune system,” Sondel says. “Specifically, if it is so strong that it can reject a liver transplant or bone marrow transplant, why can’t we use the immune system to kill cancer?”
One of the most successful immunotherapies is Chimeric Antigen Receptor (CAR) T-cell therapy, led at the School of Medicine and Public Health by Christian Capitini, MD, assistant professor, Department of Pediatrics. Only a few U.S. academic medical centers are using this therapy for children with refractory acute lymphoblastic leukemia. The technique extracts T-cells from a patient, then bioengineers them to create cancer-fighting T-cells before infusing the cells back into the patient.

Another innovative therapy is alpha beta T-cell depletion. In a protocol developed by Mario Otto, MD, PhD, and Kenneth DeSantes, MD, the patient’s immune system is destroyed through high-dose chemotherapy. Immune cells and stem cells obtained from a half-matched donor, usually a parent, are manipulated utilizing a method co-developed by Otto, an associate professor in the Department of Pediatrics. The process uses magnetic beads, which attach to a protein and “snatch” the alpha beta T-cells that cause GVHD. The remaining white blood cells and stem cells are infused into the patient, and can attack and kill cancer cells, decrease the risk of infection and restore the production of normal blood cells.
“We use this approach on patients with leukemia,” says Sondel, the Reed and Carolee Walker Professor in Pediatric Oncology. “Additionally, we’re the only center in the nation to use this approach to treat solid cancers, such as neuroblastoma, that haven’t responded to conventional treatments.
DeSantes — a professor in the Department of Pediatrics and director of the Pediatric Hematology, Oncology and Bone Marrow Transplant Program at American Family Children’s Hospital — recently opened another U.S. Food and Drug Administration-approved clinical protocol in which he takes healthy cells from a donor, grows them in the lab to “activate” them, and infuses the cells — along with an anti-cancer antibody — into a cancer patient.
Reflecting on all that has transpired since the first successful bone marrow transplants, Albertini — who earned his medical degree and doctorate at the School of Medicine and Public Health, did postdoctorate research with Bach and completed a residency at UW Health before moving to Vermont — says, “I’m proud to have Wisconsin in my background and to have worked on remarkable research with remarkable people.”
Today, immunotherapy can be considered the standard of care for certain types of cancer, leading some to ask whether bone marrow transplants will be needed at all.
“I think that procedure will become passé for cancer patients, but not for children who are born with genetic defects that cause potentially fatal diseases, in which the bone marrow malfunctions,” Sondel says, predicting that bone marrow transplants will remain relevant for several more decades.
He adds, “In theory, if the bone marrow is not working correctly because a gene is missing, you can take some of the bone marrow and insert the correct gene, then give the marrow back to the patient. It’s already happening for some diseases, such as select subtypes of severe combined immune deficiency syndrome, but we don’t know whether or when this will be possible for many other genetic diseases.”
Figuring out next steps like this is in line with the mission of the North American Pediatric Dream Team of researchers — including Sondel, Capitini, DeSantes and Otto — who have dedicated their careers to understanding the immune system and developing treatments that use its power to battle deadly diseases. Their quest continues.