“That was the second time we had done a bone marrow transplant on the (Wisconsin) patient,” notes Albertini. “The first time, we didn’t immunosuppress his system, but for the second, we completely wiped out his system to suppress it before the transplant, thereby enabling the transplant to grow successfully.”
Albertini saw evidence of the long-term success of the boy’s second transplant when the recipient — then an active teenager — visited him several years later at the University of Vermont.
About seven years after the first successful transplants, Bach found a way to speed up the MLC test so it required only several hours rather than six days. In addition to benefitting bone marrow transplant patients, the speeded-up test also positively impacted cadaver kidney transplant recipients, because that procedure must be done within 48 hours of the donor’s death.
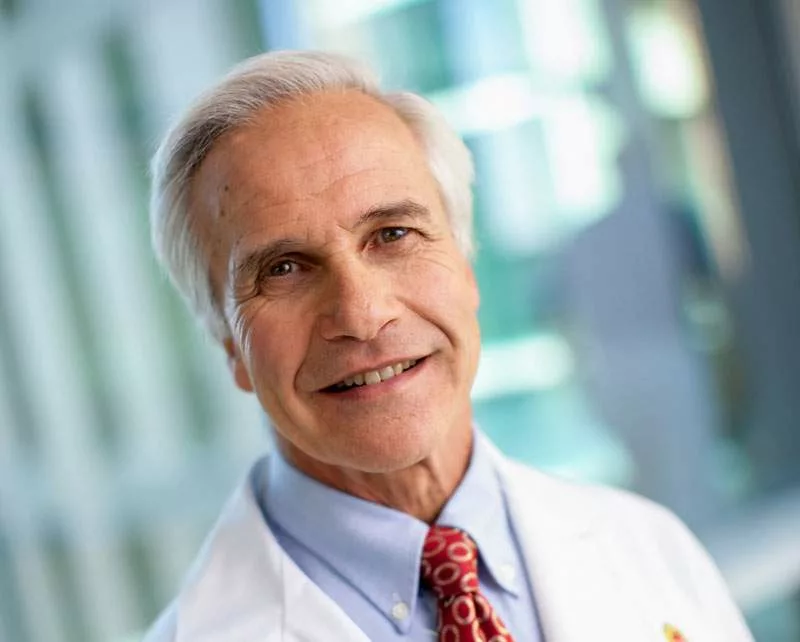
“Fundamentally, we still conduct this testing, but we have a refined way of doing so,” explains Mark Juckett, MD, director of the Adult Bone Marrow Transplant Program at UW Health and a professor (CHS) in the Department of Medicine’s Division of Hematology and Medical Oncology.
Today, bone marrow transplants can be done with unrelated donors. The National Marrow Donor Program, otherwise known as the “Be the Match” program, was founded in 1986 and includes approximately 10 million potential bone marrow donors. The registry allows physicians to conduct transplants on the 75 percent of patients who need a bone marrow transplant but who don’t have a family member who is a match.
“Hopefully, through research, bone marrow transplants will continue to get easier and safer for patients, or we will find other treatments that are less risky,” says Juckett, noting that Bach’s early work and successful transplants paved the way for five decades of advances, with more on the horizon.
Innovative Therapies Take Center Stage
When transplants were first performed for children and adults with leukemia, patients were treated with high doses of chemotherapy and total body radiation in an attempt to cure the disease. The transplant was given immediately after the chemotherapy and radiation in order to rescue the patient from a major side effect of this treatment — severe damage to the patient’s normal bone marrow.
It was later discovered that immune cells from the donor, transferred to the patient with the transplant, played an important role in destroying any cancer cells that were not killed by the chemotherapy and radiation, a phenomenon now known as the “graft-versus-leukemia” effect. This realization facilitated the development of many other immune-based therapies to fight cancer.
“We’re at the beginning of new types of therapies in which patients are given cells using novel techniques,” Juckett says, referring to immunotherapies that use the body’s own white blood cells to kill leukemia and other cancers without destroying normal tissue.
Sondel has pored over the concepts behind immunotherapy for five decades.
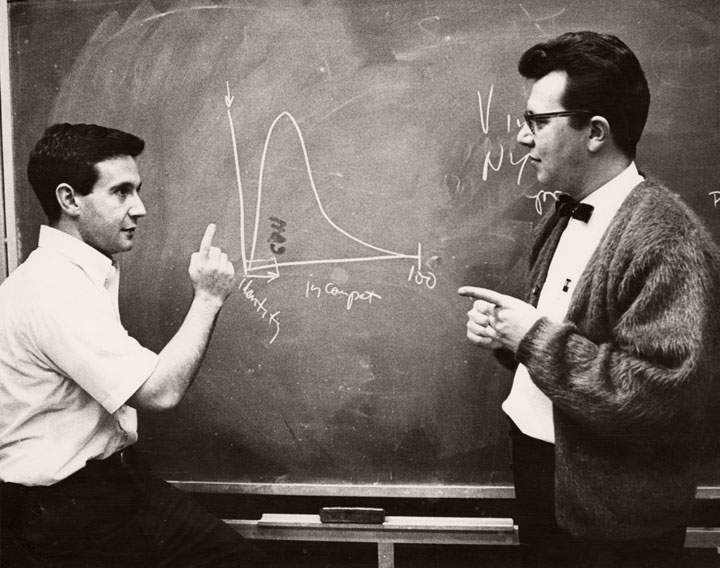
“I remember, back in 1969, talking with Fritz Bach about the strength of the immune system,” Sondel says. “Specifically, if it is so strong that it can reject a liver transplant or bone marrow transplant, why can’t we use the immune system to kill cancer?”
One of the most successful immunotherapies is Chimeric Antigen Receptor (CAR) T-cell therapy, led at the School of Medicine and Public Health by Christian Capitini, MD, assistant professor, Department of Pediatrics. Only a few U.S. academic medical centers are using this therapy for children with refractory acute lymphoblastic leukemia. The technique extracts T-cells from a patient, then bioengineers them to create cancer-fighting T-cells before infusing the cells back into the patient.