Kathryn Budzak
Since medical school, Kathe Budzak has aimed to bolster the close-knit feeling among her classmates by writing letters and encouraging attendance at gatherings.
Lincoln Ramirez, MD, PhD, had an idea for a laboratory in which neuroscientists of all ages could “acquire the vision needed to navigate the brain and all its great tributaries.” He knew that only by repeated dissections of our body’s most complex organ could the neurosurgeons of the future learn to care for the patients of the future.
Today, students who enter the new lab walk by a displayed quote from Ramirez, emeritus professor, Department of Neurological Surgery, University of Wisconsin School of Medicine and Public Health (SMPH), that says, “The study of the brain is a privilege, and the practice of neurosurgery is an honor.”
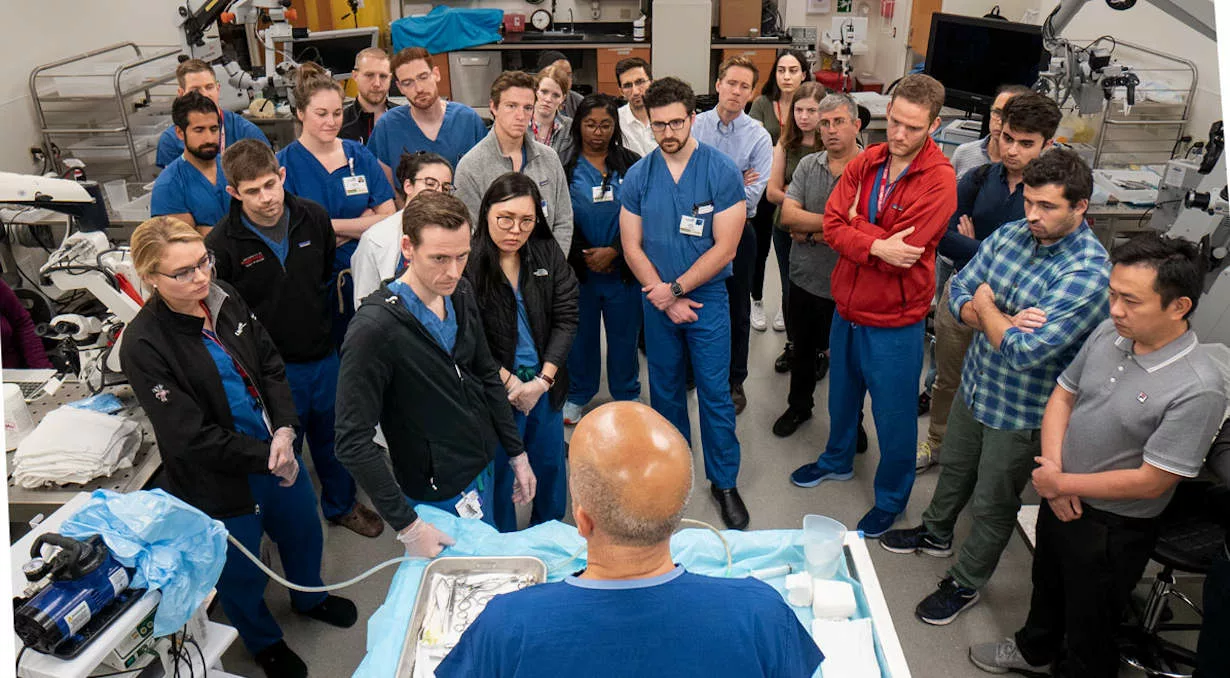
The Lincoln Ramirez Neurosurgery Operative Skills Laboratory, which opened in University Hospital’s K Tower in late 2018, is fulfilling its mission and already has been the source of about two dozen research papers. In addition to research and teaching, the lab serves as the centerpiece for surgical skills courses focused on techniques used for micro-neurosurgery, and cranial, spinal and peripheral nerve surgery.
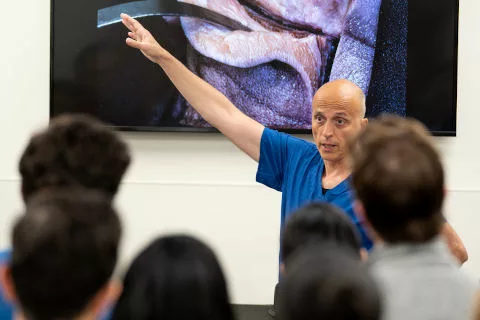
Surgeon Mustafa K. Baskaya, MD, laboratory director and professor, Department of Neurological Surgery, teaches a series of courses that bring neurosurgery residents and fellows from all over the United States to learn microvascular surgery techniques and the best approaches for skull-base, cerebrovascular and complex brain tumor surgeries. Baskaya is an expert in these approaches, which allow surgeons to access the brain through the nose, mouth and other points at the base of the skull to spare as much healthy brain tissue as possible. He also teaches classes geared toward SMPH medical students and UW Health residents.
Additional faculty members who teach in the lab include several from the Department of Neurological Surgery—Nathaniel Brooks, MD (PG ’09), associate professor, who uses the lab for a spinal surgery class; Amgad Hanna, MD, associate professor, who teaches peripheral nerve surgery techniques; and Azam Ahmed, MD (PG ’10), assistant professor, who teaches endoscopic skullbase surgery — as well as the Department of Surgery’s Division of Otolaryngology–Head and Neck Surgery — Ian Koszewski, MD (PG ’17), assistant professor, Joseph Roche, MD, assistant professor, and G. Mark Pyle, MD ’84, professor, who teach skullbase surgical approaches.
“The laboratory’s approach makes it one of the more productive in the world and fully embraces the completeness of the teaching mission,’’ says Robert Dempsey, MD, the Manucher Javid Professor and Chair of Neurological Surgery and a longtime leader in global neurosurgical education. “What we teach is how to improve your medical and surgical knowledge. This is the root of outstanding neurosurgical clinical care and has drawn interest from trainees not only from the region, but also the nation and the world.” Illustrating this point, a map on the laboratory wall features push pins indicating the places where neurosurgery researchers came from, including various cities around the United States, as well as Australia and China, with a forest drawn in Turkey, the country of origin for Baskaya and Burak Ozaydin, MD, laboratory manager. Famed neurosurgeon Mahmut Gazi Yasargil, MD, considered the father of modern microneurosurgery, also was born in Turkey.
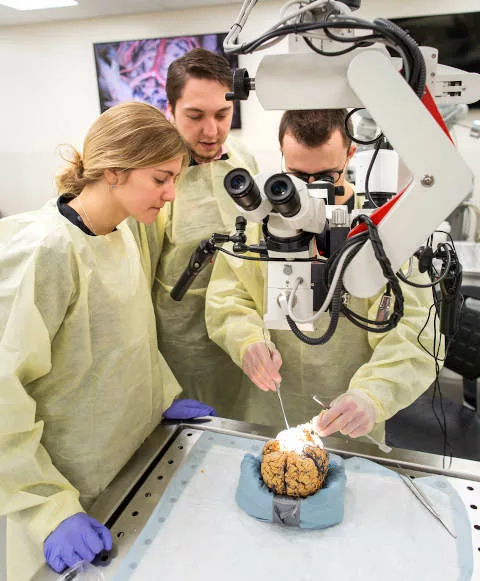
Early in 2019, one of only two neurosurgeons in Chad, population 15 million, trained in this laboratory, and during that summer, residents and fellows doing research in the laboratory were from Turkey, Argentina, Iran, Egypt and China. Some worked on ultra-microsurgery techniques, using sutures as fine as hair, to be able to bypass vessels blocked by ischemic strokes or ruptured by hemorrhages.
Among that group, Santiago Feldman, MD, a senior resident of neurosurgery from Argentina, was working on a cadaver skull in the tricky location around the parotid gland, which is traversed by the carotid artery and facial nerves, as well as many other nerves.
“This is a very difficult area; it is very complex and can be confusing for students. You can’t comprehend this region from a book. To be able to conceptualize this area three-dimensionally, you need to see, touch and dissect a real specimen,” describes Ozaydin.
For learners, the laboratory has eight tables with downdraft air flow, an important factor because otherwise “you wouldn’t be able to work in here for long,” due to the overwhelming odor of formalin used to preserve the skulls, he explains.
Able to accommodate trainees in up to 16 stations, the laboratory also allows video recording in two and three dimensions and features two large display screens on which students can watch a magnified view of dissections and other lessons. While wearing three-dimension glasses, students can see an enhanced view of deep brain structures.
During summer 2019, Ozaydin and other neurosurgeons conducted a brain anatomy course for more than 20 nurses who care for patients following strokes and other brain injuries in the Neuroscience Intensive Care and Acute Care Units at University Hospital, and the Neurosurgery and Neurology Clinics. At one station, Feldman showed the location of blood vessels that are often involved in stroke. At another, Jian Ruan, MD, an attending neurosurgeon from China, demonstrated the endonasal approach to surgeries involving pituitary tumors and other skull-base tumors, while projecting on the large screens endoscopic images from that part of the brain. Andrea Strayer, MS, NP, CNRN, a nurse practitioner who cares for patients on University Hospital’s acute neurosurgery floor, says the knowledge she and others gained during such lessons translates directly to patient care.
“It is so vital for us to have this knowledge, it helps in communicating with patients,’’ says Strayer, who also helped organize a spinal-anatomy class for nurses. “We are part of a big, complicated neurosurgery team, and nurses play an important role. Nurses don’t have opportunities for this type of class in most places, so it’s a wonderful opportunity for us.”
While all lessons taught in the lab are important, perhaps the most profound is the story behind a photo of the Schumacher family, of Appleton, Wisconsin, which Baskaya prominently displays in the lab.
Baskaya cared for Bob Schumacher when he was diagnosed with a brain tumor, and Bob’s wife, Melissa Schumacher, believes Baskaya’s surgical skills allowed her husband to have a better quality of life and live longer than he otherwise would have, which gave him time with the couple’s daughter, Riley. The Schumacher family and many other grateful patients helped pay for the lab through donations.

“Delivering the best care to our patients is the whole reason we are constantly trying to improve our techniques and approaches to neurosurgery,’’ says Baskaya. “The photo of the Schumacher family reminds us why we are here.”
While the lab certainly impacts patients at University Hospital, its international focus helps improve outcomes for neurosurgery patients around the globe.
“It is our duty to spread these microsurgical techniques worldwide,’’ says Baskaya. “Spreading this teaching globally will eventually enhance neurosurgical care for thousands of patients.”
Dempsey concurs, saying that the laboratory exemplifies the Wisconsin Idea.
“This is exactly the purpose of our major research institution: providing the very best of neurosurgical care while constantly working on ways to improve that through surgical research, which will benefit patients far into the future,” Dempsey concludes.