Welcome, Dean Ahuja!
On May 15, Nita Ahuja, MD, MBA, became the 10th dean of the University of Wisconsin School of Medicine and Public Health (SMPH) and vice chancellor for medical affairs at UW–Madison.
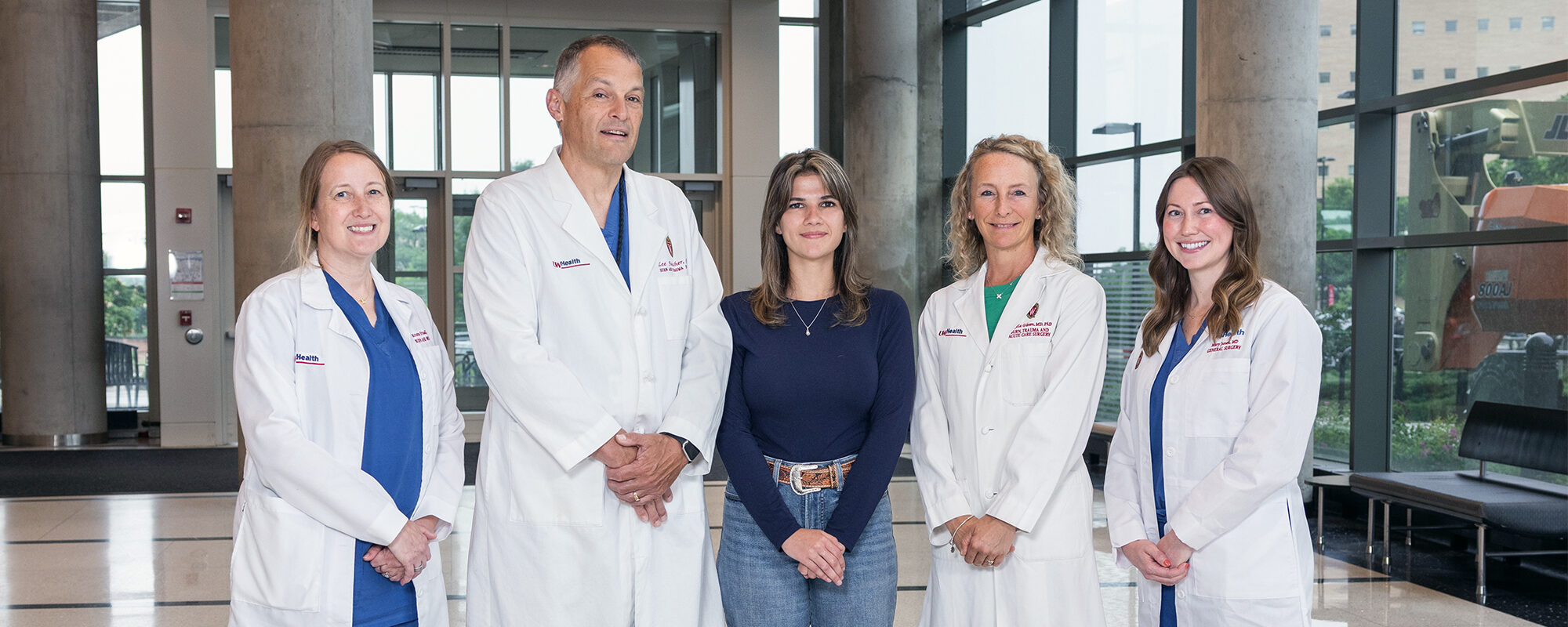
Left to right: Kristin Friedl, RN, DNP, ACACNP-BC; Lee Faucher, MD ’96; patient Ryen Reif; Angela Gibson, MD ’09, PhD ’07 (PG ’14, ’15); and Mary Junak, MD, gather near the entrance to the Wisconsin Institutes for Medical Research in June 2025.
When Ryen Reif was transported to University Hospital in February 2024, she could only focus on the short-term. “All I was worried about was calling off work,” she recalls. “I was like, ‘Oh, my God. I’m going to have to call my boss and say I can’t work tomorrow.’”
Reif’s legs were badly burned following a bonfire accident. She had been transferred to the UW Health Burn and Wound Center from Janesville, Wisconsin, unaware of how her injuries would impact her life.
“When I got there, they’re like, ‘Oh, honey, it’s going to be more than a few days,’” Reif recounts. “I didn’t realize it was as bad as it was until I talked to the nurses.”
Reif, then 19 years old, spent about three weeks in Madison under the watchful care of the burn team, with “team” being the operative word. She received care from surgeons, nurses, physical therapists, social workers, dieticians, pharmacists, and more, all dedicated to helping her return to the comforts of home and her job as a paraprofessional at Marshall Middle School in Janesville.
“Burn is the most, in my opinion, multidisciplinary specialty that you can [participate in],” says Kristin Friedl, RN, DNP, ACACNP-BC, nurse practitioner, Division of Acute Care and Regional General Surgery, Department of Surgery, University of Wisconsin School of Medicine and Public Health (SMPH); she adds that good patient outcomes require the involvement of every team member.
Friedl holds three degrees from UW–Madison (bachelor’s degrees in communicative disorders and nursing and a doctorate of nursing practice) and is a veteran of 18 years in the burn unit. Thus, she is well-versed in the collaborative nature of the care provided.
Angela Gibson, MD ’09, PhD ’07 (PG ’14, ’15), associate professor, Division of Acute Care and Regional General Surgery, and medical director, UW Health Wound Healing Services, also has deep roots at UW–Madison. Gibson started by earning her bachelor’s degree in nursing, during which she worked as a student nursing assistant in the burn unit. Upon graduation, she began working as a nurse in the burn unit and ultimately decided to enroll in SMPH’s Medical Scientist Training Program; in that program, she earned her medical and doctoral degrees, with the goal of becoming a burn surgeon–scientist. She completed a general surgery residency and critical care fellowship at University of Wisconsin Hospital and Clinics. In 2015, she joined the SMPH Department of Surgery as a full-time faculty member.
It was during Gibson’s time as an undergraduate that she recognized the close-knit nature of the burn team.
“I really loved the community of the burn team,” she reflects. “I felt like such a part of a team even as a student nursing assistant.”
That sense of team translates into extraordinary patient care. In 2006, the American Burn Association first verified the UW Health Burn and Wound Center. Attaining this rigorous verification serves as a mark of excellence, as it demonstrates that a center offers the highest quality care for burn and wound patients from the time of injury through rehabilitation.
The Burn and Wound Center also is a Level I Trauma Center, as verified by the American College of Surgeons, indicating the highest level of trauma care available in the United States. It is the only Wisconsin center to carry that distinction for both pediatric and adult patients.
A dedication to the service of others is true across the varied disciplines of care provided by faculty and staff at the Burn and Wound Center, who say they are able to forge unique relationships with patients due to the nature of the care they provide.
“It is a lifelong injury with lifelong complications from a physical and a mental standpoint,” Gibson says. “Being able to partner with patients for that entire journey is very rewarding. It takes the whole team to get them through because there are so many aspects of their treatment.”
Those special connections can manifest themselves in special ways, such as invitations to weddings after patients recover. Friedl tells the story of a patient who runs a farm and makes weekly visits to the unit to bring fresh eggs and maple syrup for the staff and patients. His wife also makes blankets for pediatric patients.
“A lot of burn patients, we’ll know them for many years after their injury, if not their whole life,” she says. “We develop a really close relationship with them and get to know them as people.”
For instance, during Reif’s stay in the Burn and Wound Center, she experienced that connection firsthand. Lee Faucher, MD ’96, professor, Division of Acute Care and Regional General Surgery, and medical director, UW Health Burn and Wound Center, was the lead surgeon on Reif’s case.

“Her surgeon, Dr. Faucher, was amazing,” says Reif’s mother, Tricia Reif. “He understood Ryen and her sense of humor. She always looked forward to his visits, and I think he gave her a level of comfort.”
That admiration went both ways, according to Faucher.
“Ryen was beyond her years in the way she handled this very difficult, serious injury,” he notes. “She never placed blame anywhere. She did everything she needed to get through this very difficult ordeal.”
During her time in Madison, Reif also benefited from the help of participants in the Survivors Offering Assistance in Recovery Program, which offers an opportunity for burn survivors to counsel recent burn victims, share their experiences, and offer much-needed perspective. Reif is training to join the program, with the goal of giving back.
“At first I thought I would just hash [my injury] out on my own because I like to think I’m very independent,” she shares. “But a gentleman I know, who is a friend of a friend, was up on the burn unit a week or so after I was, and I got to meet him and talk to him. We had so many similar experiences at the hospital. It just felt really great to be able to talk to somebody who knew what I went through.”
Reif continues, “I want to be able to give people what I got from that experience, which was a sense of reassurance. There are other people who know this pain and have persevered through it.”
Five years ago, UW Health unveiled a nearly $6 million upgrade to the Burn and Wound Center that enhanced the ability of the team to care for patients; a portion of the improvements relied upon the generosity of donors. The center expanded from seven to 11 beds, with each room having a private shower. An additional tub room was added, offering more space for patients to have their burns washed. Burn washing is one of the most important processes in patient recovery, and those upgrades have paid huge dividends.
“Patients are not always completely healed when they go home, so being able to give them the autonomy and confidence to be successful in their wound care before we send them home is empowering,” Gibson explains.
Upgrades also have allowed for a clearer path to emotional healing. For instance, each room is equipped with a pullout couch to allow families the option of staying with their loved ones.
“Our patients are sometimes here for 60 days, so this can become home for some families,” Faucher says. “Having a support person with the patients, when they’re here that long, is very important.”
A renovated playroom for children offers convenient options for pediatric patients or siblings. An enhanced physical therapy/occupational therapy gym provides greater opportunity to mimic conditions that patients will experience when they leave the hospital.
“One of the main things they made sure I knew how to do was my own wound care,” Reif says. “They even showed my parents how to do it, in case I needed help. And they asked me questions about my home life. Do you have stairs? Is your bedroom upstairs? If I could not do something, they gave me a lot of solutions to the problems I may have had at home.”
Faucher states, “Recovery is a long, intensive process. The new space is a physical complement to the research and direct medical care we provide, and it allows us to offer equipment that burn patients require to recover.”
Gibson, Faucher, and Friedl are all products of training at UW–Madison and have helped the burn program grow. Each plays a role in molding the next generation of surgeons.
“One of my favorite things about working in the burn center is that we attract such high-quality residents and medical students,” Friedl notes. “They are absolutely amazing. They’re such hard workers. They’re eager to learn, and it’s wonderful having them on service.”
One such individual is Mary Junak, MD, a third-year general surgery resident who recently completed two years of research in Gibson’s lab. Her time working on the burn team has influenced her desired career path.
“We do the rotation as an intern, and there’s no senior resident,” says Junak. “I feel like it is a rotation in which you can really take ownership of the patients. The advanced practice providers we work with are amazing. They have so much information and are good at teaching.”
According to Gibson, the introduction to burn and wound care early in a resident’s career is purposeful due to the nature of the care.
“It provides a lot of foundational knowledge for trainees on how to diagnose different wounds,” Gibson says. “No matter what subspecialty they go into, they will have baseline experience in wound healing, which is critical.”
In addition, trainees gain valuable experience in patient care and how to practice with autonomy.
“Medicine is changing every day, but there are still steadfast rules that I hope will never change — that physicians always need to deliver compassionate, patient- and family-centered care,” Faucher observes. “They must be able to explain things so the patient fully understands and can actively participate in their care.”
The team atmosphere and collaborative aspect of the burn unit apply to all of its missions, including education. Faculty and advanced practice providers are deeply invested in the success of trainees.
“Dr. Gibson has been my biggest mentor. She has been very supportive and encouraging,” Junak says. “She is enthusiastic and passionate about what she does, and I think that makes other people really care about it.”
Junak continues, “Dr. Faucher also has been really supportive and helped me think about what kind of fellowship programs I am interested in. How much burn care do I want to do? How much trauma? How much critical care? He has helped me talk about fellowship plans and connect me with program directors.”
The one constant during Friedl’s nearly two-decade career in the burn unit has been growth. The burn doctors and scientists are constantly researching new ways to help burn patients.
“In burn, there is always something new coming around the bend, and as a nurse practitioner, I have a role in helping build new processes when new products come to market,” Friedl shares.
Gibson spearheads much of that innovation through the work in her lab. Advances include things like evaluating skin substitutes for faster treatment and less scarring, and understanding how the depth of a burn injury impacts healing. Typically, treating a burn involves skin grafting, a procedure that takes healthy skin from a “donor site” on a patient’s body and transplants it to the burn area. Gibson hopes to minimize the need for that process by better understanding the skin in the wound.
“We have been cutting away viable tissue because we were unable to detect that with our visual evaluation,” she explains. “Maybe if we left some of that at-risk tissue, we could actually get the patient to heal on their own or at least heal with less of a donor site. With this approach, we have seen less scarring while reducing the pain that a patient has to go through.”
Research, education, and collaboration all support tremendous patient care, which is what the UW Health Burn and Wound Center and its team hold as a source of pride.
“Having a patient walk out of the hospital as functional as they can possibly be so they can get back to their normal life, to me that is the most amazing part of the burn center,” Friedl states. “And that only happens because everyone on the care team is valued, because their piece truly matters.”